Post-COVID Care and Treatment, The Road to Recovery
The unexpected and intrusive arrival of COVID-19 has changed the way we live our lives. The disease’s unprecedented nature and scope have left many of us wondering how we will rebuild our futures in a post-COVID world. COVID survivors face a more significant challenge as the potential long-term complications and prolonged symptoms create uncertainty and fear. As communities prepare to return to normal, COVID survivors are tinged with concerns about life beyond lock-down.
BACKGROUND
Coronaviruses are a large family of viruses that cause respiratory infections ranging from the common cold to more severe diseases. COVID-19 is a disease caused by a new form of coronavirus, and symptoms range from mild illness to pneumonia. While some recover quickly, others may get very sick and have persistent respiratory symptoms such as coughing, sore throat and shortness of breath following COVID-19. Whether COVID survivors recover spontaneously or have delayed recovery, our advice for post-COVID care strategies will support people living with symptoms affecting their everyday life.
REST
Patients recovering from COVID-19 should focus on managing their energy. Post-viral fatigue is expected during the recovery phase and may range from feeling tired to extreme exhaustion. Fatigue is the body’s normal response to fighting a viral infection, so it is essential to rest the body and mind while it recovers. Relaxation and meditation can help support quality rest. Fragrances, blankets, and soothing music may promote deep relaxation and improve your mood. Avoid physical and emotional exhaustion by keeping television, social media, and phones to a minimum. As your fatigue improves, continue to take short breaks throughout the day and calm your mind with relaxation techniques.
ACTIVITY
Keep activity levels low and only do a small number of activities throughout the day. Basic activities of daily living such as washing and dressing may be taxing, so move slowly and gently. As your fatigue lifts, you may want to gradually incorporate a light amount of activity in your day with periods of regular rest. Avoid increasing activity levels too quickly and pushing through fatigue which can set you back. Be realistic about what level of activity is manageable, and be kind to yourself as you recover.
NOURISHMENT
Our bodies require more energy and fluids while fighting an infection. Do your best to maintain a routine with eating and drinking to support your immune system during recovery. Make the most out of your food and drink by choosing higher protein options to give your body the extra energy it needs. If you find that you have a poor appetite, talk with your provider about supplementing the short-term with a high calorie and protein drink to give your body the energy it requires. You may find that eating little and often and taking smaller bites while taking deep breaths makes it easier to consume food. Rather than eating three large meals, opt for snacks throughout the
day that you find appetizing. To cope with changes in taste and smell, try consuming sharp, spicy, or sugary foods with stronger tastes. If you cannot make it to the grocery store, contact your local grocer to ask about pickup and delivery services so you can get back to everyday life sooner.
BREATHING CONTROL
Manage breathlessness by practicing breathing control. Breathing control is when you breathe gently, using little effort. When you feel suddenly short of breath, slowly breathe in through your nose with your mouth closed, so air reaches deep in your lungs. Your stomach should rise as you breathe in. Breathe out through your nose, allowing your stomach to fall gently. Try to use minimal effort to make breaths slow, relaxed and smooth. Rest and wait for each new breath to come. If your blood oxygen levels are persistently low, you may require supplemental oxygen. Oxygen therapy is not a treatment for breathlessness but is an effective at-home treatment for low blood oxygen saturation.
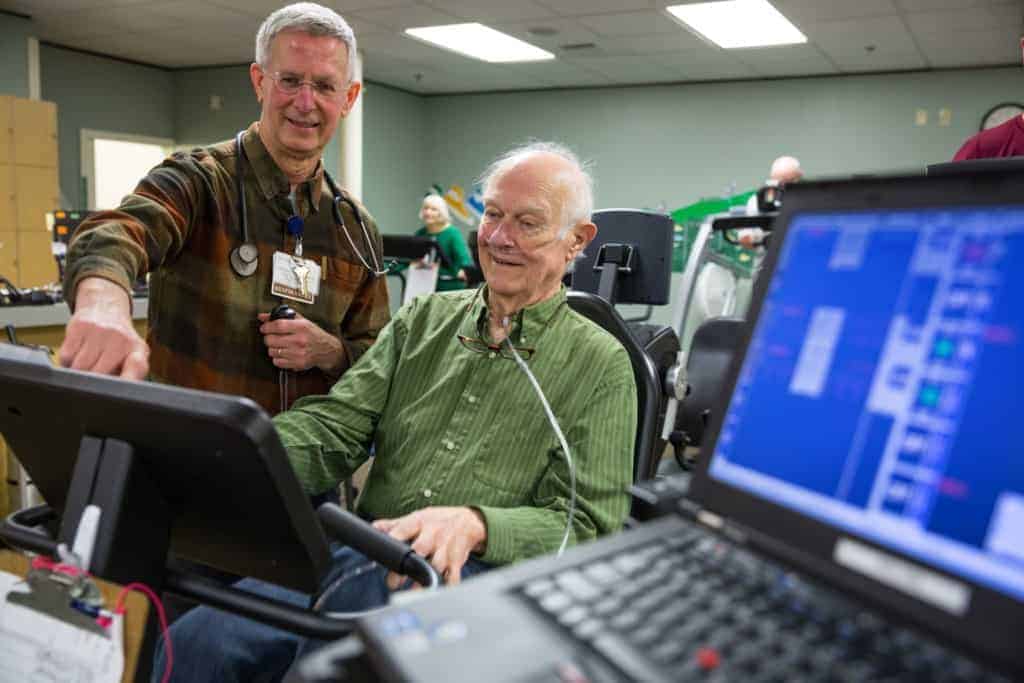
REHABILITATION
Your provider may discuss pulmonary rehabilitation or physical/occupational therapy outpatient care to help manage prolonged symptoms as part of your recovery. This may include standard diagnostic evaluations, including pulmonary functions tests, physical function assessments and repeat imaging scans. Current research suggests that rehabilitation plays a crucial role in recovery. Using a combination of at- home exercise plans and outpatient therapy sessions, patients find relief from persistent symptoms, including shortness of breath, chest pain, cough, fatigue, and joint pain. Your provider will coordinate subsequent care to meet your specific needs during recovery.
MENTAL HEALTH
Being ill for a long time can impact your mental health. While recovering from COVID, you may feel anxious, depressed, afraid, or frustrated. If your recovery is taking longer than expected, you may become easily irritated or angry. Try distracting yourself by going for a walk, listening to a podcast, or calling a friend when feelings of anxiousness arise. Slowly increase your activity level and do things that make you happy such as gardening or walking your dog. Stick to a good sleep routine, so your body has time to repair itself. Try to go to bed and wake up at roughly the same time every day to help reduce irritability and boost your mood. By incorporating a few mental wellbeing activities each day, you will see significant improvements and feel a sense of accomplishment.
LONG COVID
Long COVID refers to patients who have recovered from the initial stages of the COVID-19 illness but experience many symptoms well beyond the initial infection. Symptoms may include shortness of breath, fatigue, fevers, gastrointestinal symptoms, sleep disorders, memory and concentration problems, anxiety, and depression. These symptoms can persist for months past the initial recovery phase and can range from mild to severe. Unfortunately, new symptoms may arise well past the time of infection or evolve into new symptoms altogether.
According to the Centers for Disease Control and Prevention (CDC), 35-54% of patients with mild acute COVID-19 experienced persistent symptoms two to four months beyond the immediate illness. Research into the prolonged health consequences of COVID-19 is rapidly evolving, and medical professionals are working diligently to find ways to treat and prevent these widespread and lasting symptoms. A global effort is underway to develop centers dedicated to research long COVID and how best to care for those who have it.
SLOW THE SPREAD
Whether you recover quickly from COVID or take much longer, it is essential to work with your healthcare provider on an individualized management plan to support recovery. Keep in mind that having COVID-19 does not grant complete immunity to the illness. While cases of reinfection are rare, it is best to take steps to protect yourself and others. Continue wearing a mask in public places, stay at least 6 feet away from others, wash your hands with soap and water often, and avoid crowds in confined areas. Teach your immune system how to recognize and fight the virus by getting the COVID-19 vaccine. If you have questions about getting vaccinated, a conversation with your provider might help put your mind at ease.

John Mathis, MD is a board certified internal medicine provider at Fidalgo Medical Associates. He attended medical school at University of Utah followed by a residency at Virginia Mason Medical Center. His professional interests include pulmonology, cardiology and critical care. For more information or to schedule an appointment with Dr. Mathis, call Fidalgo Medical Associates at 360-293-3101.
Published on June 25, 2021
